Editor’s note: Elmore described her own cancer-misdiagnosis experience in this video.
The latest guidelines for the diagnosis of skin cancer provide for a more accurate diagnosis, but still allow for a great deal of error, says a study published today in the new journal JAMA Network Open.
“Providing a diagnosis on skin biopsies can be challenging. A biopsy might be interpreted differently if a second or third pathologist is asked to review the case,” said Dr. Joann Elmore, lead author. She is an adjunct professor of medicine at the University of Washington School of Medicine and professor at the David Geffen School of Medicine at UCLA.
Elmore knows this firsthand. A decade ago, three pathologists reviewing Elmore’s own skin biopsy provided three different opinions, including an erroneous diagnosis of melanoma.
“There is a lot of uncertainty in medicine that is often forgotten by both health care providers and patients,” she said. “These latest findings underscore the need to inform patients that a diagnosis can be imperfect. And we need to find a better way to diagnose both harmless lesions and invasive melanoma.” Invasive melanoma kills more than 9,000 Americans a year.
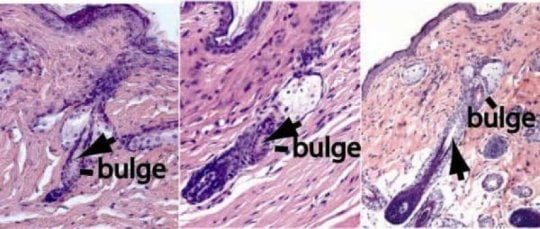
The challenge is that melanoma is diagnosed by visual interpretation. Every year, millions of Americans have a suspicious mole or skin lesion biopsied and sent to a pathologist to determine whether it is a potentially deadly melanoma. The pathologist examines a slide of a thin slice of tissue and compares what is seen to published guidelines for what is cancer and what is not.
The pathologist’s interpretation is thus crucial to what happens next for the patient. If the lesion is diagnosed as benign, no treatment may be recommended. But if the pathologist says the slide suggests malignancy, the patient will typically undergo surgery and perhaps other treatments.
Pathologists are likely to agree when lesions are clear-cut – either benign or highly malignant – but they often disagree when interpreting lesions in the middle range.
Elmore and colleagues first published a paper on this challenge last summer. The American Joint Committee on Cancer has since issued new guidelines for staging of melanoma.
In the new paper, the researchers describe what happened when the old guidelines and the latest guidelines were applied to more than 4,300 individual slide interpretations examined by 187 pathologists in several states. The study found that pathologists agreed with an expert reference diagnosis on the status of 54 percent of early-stage invasive melanoma, versus 44 percent using the older guidelines. For cases diagnosed as a late stage of invasive melanoma, the pathologists agreed on 78 percent of the samples versus 72 percent under the earlier guidelines.
The study calls the improvement “modest,” but scientists are considering ways to improve diagnostic tools.
In the 2017 report, Elmore wrote, “The diagnostic variability that we found does not mean that pathologists are the problem. My appreciation of the challenges pathologists face on a daily basis attempting to classify biopsy specimens has grown exponentially. Interpreting these lesions is especially difficult and carries a lot of responsibility. Pathologists embrace this responsibility with the utmost skill and thoughtful commitment.”
Collaborators on the paper include senior author Dr. Michael Piepkorn, clinical professor of medicine, Division of Dermatology, at the UW School of Medicine.
[“Source-newsroom”]