Table of Contents
ToggleAbstract
The treatment of alopecia is limited by a lack of therapies that induce and sustain disease remission. Given the negative psychosocial impact of hair loss, patients that do not see significant hair restoration with conventional therapies often turn to complementary and alternative medicine (CAM). Although there are a variety of CAM treatment options on the market for alopecia, only a few are backed by multiple randomized controlled trials. Further, these modalities are not regulated by the Food and Drug Administration and there is a lack of standardization of bioactive in gredients in over-the-counter vitamins, herbs, and supplements. In this article, we provide a comprehensive review of the efficacy, safety, and tolerability of CAM, including natural products and mind and body practices, in the treatment of hair loss. Overall, there is a need for additional studies investigating CAM for alopecia with more robust clinical design and standardized, quantitative outcomes.
Introduction
According to the National Center for Complementary and Integrative Health (NCCIH), a branch of the National Institutes of Health (NIH; Bethesda, MD, USA), more than 30% of adults and 12% of children utilize treatments developed “outside of mainstream Western, or conventional, medicine,” with a total USD 30.2 billion out-of-pocket dollars spent annually [1]. In the treatment of alopecia, there is an unmet need for therapies providing satisfying, long-term results. Patients often turn to complementary and alternative medicine (CAM) in an attempt to find safe, natural, and efficacious therapies to restore hair. Although CAMs boast hair-growing potential, patients may be disappointed with results as there is a lack of standardization of bioactive ingredients and limited scientific evidence.
Multiple factors contribute to hair loss, including genetics, hormones, environmental exposure, medications, and nutrition. Treatment of hair loss requires a multimodal approach and the use of CAM may provide added benefits. Vitamins and trace minerals are vital to the hair follicle cycle and maintain homeostasis as enzyme cofactors, hormones, antioxidants, and immunomodulators. Botanical products regulate inflammation, minimize oxidative stress, and control hormone levels (i.e., dihydrotestosterone). Beyond supplementation, mind and body practices, including acupuncture and massage, help to reduce physiologic and emotional stress, which may contribute to hair loss.
Complementary and Alternative Medicine
Complementary medicine refers to practices used concomitantly with conventional therapies, while alternative medicine is used in place of these therapies. The NCCIH divides CAM approaches into three main categories: (1) natural products; (2) mind and body practices; and (3) other (i.e., homeopathy) [1]. CAM provides the option to choose promising, low-risk, adjuvant and alternative therapies. Herein, we provide a comprehensive review of CAM treatment options for alopecia, with most evidence in androgenetic alopecia (AGA) and alopecia areata (AA). Table 1 provides an in-depth summary of these investigations.
Summary of clinical investigations on complementary and alternative treatments for alopecia
Natural Products
Natural products encompass a variety of subgroups including vitamins and minerals, herbs/botanicals, and probiotics, all of which are globally marketed as dietary supplements and do not require Food and Drug Administration (FDA) approval. The 2012 National Health Interview Survey reports natural products to be the most popular CAM approach for dermatologic conditions, used by 17.7% of Americans [2, 3]. Data is available for the use of amino acids, caffeine, capsaicin, curcumin, garlic gel, marine proteins, melatonin, onion juice, procyanidin, pumpkin seed oil, rosemary oil, saw palmetto, vitamin B7 (biotin), vitamin D, vitamin E, and zinc to treat hair loss.
Amino Acids
A variety of amino acids have been studied for the treatment of hair loss. Most notably, cystine and lysine have been evaluated in humans. Other amino acids, including methionine and arginine, are often included in hair nutraceuticals, but have not yet been evaluated in clinical studies.
Cysteine plays a central role in hair health; it forms dimers that are oxidized to produce cystine, creating disulfide bridges that provide strength and rigidity between keratin strands. In disorders with decreased cysteine, such as trichothiodystrophy, there is a deficiency of sulfur containing amino acids, and hair is brittle [4]. In homocystinuria, patients have thin and hypopigmented hair [5]. Many nutraceuticals contain cysteine rather than cystine, in particular N-acetyl-L-cysteine (NAC), as it is better absorbed than any other cysteine product [6-8].
Oral L-cystine (70 mg) in combination with retinol was evaluated for the treatment of diffuse alopecia, with increases seen in both hair density and anagen rate [9]. Oral L-cystine (unknown dose) was also studied in combination with histidine, copper, and zinc taken 4 times daily, resulting in a significant mean change in total hair count after 50 weeks (29 vs. 11% for placebo) in 24 patients with AGA [10]. Millet seed containing amino acids, silicic acid, several B vitamins, and dietary minerals including manganese in combination with L-cystine (2 mg), and calcium pantothenate (Priorin®; Bayer Inc., Mississauga, ON, Canada) taken twice daily for 6 months showed a significantly increased anagen rate in 40 female patients [11]. Supplementation with L-cystine (20 mg), medicinal yeast, pantothenic acid, thiamine, keratin, and para-aminobenzoic acid (Pantogar®; Merz Pharmaceuticals GmbH, Raleigh, NC, USA) in 30 women with telogen effluvium (TE) resulted in significant improvement and normalization of the mean anagen hair rate after 6 months compared with placebo [12].
Lysine is an essential amino acid found in meat and eggs, and is thought to play a role in the absorption of iron. In patients with chronic TE, supplementation with L-lysine (1.5 g), iron (72 mg), vitamin B12, vitamin C, biotin, and selenium (Florisene®; Lambers Healthcare Ltd, Kent, UK) resulted in a significant 39% reduction in hair shedding after 6 months, as well as a significant increase in serum ferritin levels in women who had previously failed with iron supplementation alone [13].
Methionine is another essential amino acid that is vital for both keratin and procollagen synthesis. Studies have suggested a role for L-methionine in slowing the onset of grey hair in an in vitro model by counteracting hydrogen peroxide-mediated oxidative stress and blunting of methionine sulfoxide repair. Currently, there are no in vivo studies in human subjects demonstrating a benefit for the treatment of hair loss [14].
Arginine is a nonessential amino acid that is protective against the negative effects of hydrogen peroxide on hair proteins and hair surface lipids secondary to oxidative coloring or bleaching [15]. However, there are no studies that support arginine supplementation for the treatment of hair loss. Overall, the data regarding the use of amino acids to treat hair loss is limited. All of the trials reviewed here combined amino acids with various other supplements. Thus, no definitive conclusions can be drawn regarding the effect of amino acids on hair loss.
Caffeine
Caffeine is an alkaloid methylxanthine and functions as a phosphodiesterase inhibitor, promoting cellular proliferation. In vitro studies report that caffeine counteracts the inhibitory effects of testosterone on hair growth, promotes hair shaft elongation, prolongs anagen duration, and stimulates hair matrix keratinocyte proliferation [16]. Caffeine also downregulates testosterone-induced transforming growth factor (TGF)-β1 expression, a hair growth inhibitor, and increases expression of insulin-like growth factor (IGF)-1, a hair growth promoter. Female hair follicles appear to have a higher sensitivity to caffeine [17].
Research has focused on the use of topical caffeine for the treatment of AGA. Six months of daily caffeine shampoo use (Alpecin caffeine shampoo C1, unknown concentration, 7 mL, left on scalp for 2 min) resulted in fewer hairs extracted on the hair-pull test and hairs shed during combing, with reduced speed of hair loss progression and overall hair loss intensity [18-20]. Caffeine lotion (unknown concentration) has also been tested with similar results, including decrease in hairs released during the hair-pull test and positive treatment response in 75% of patients at 2 months and 83% at 4 months [21]. Comparison of 0.2% caffeine topical liquid to 5% topical minoxidil (MXD) demonstrated noninferiority (n = 210) with 10.59% improvement in anagen ratio compared to 11.68% using MXD (p = 0.574) [22].
Topical caffeine has also been studied in combination with conventional therapies. A topical solution containing both caffeine and 2.5% MXD was compared to 2.5% MXD alone in 60 patients with AGA. After 120 days of treatment, the combined solution was more effective than MXD alone, with 58.33% of patients satisfied versus 41.37% in the MXD cohort [23]. Another topical solution containing 1% caffeine, 5% MXD, and 1.5% azelaic acid was more effective for hair regrowth and decreased shedding after 32 weeks of treatment compared to 5% MXD alone or placebo [24]. Topical caffeine shows potential as a CAM for hair loss; however, studies are limited by lack of quantitative, standardized evaluation [18, 19, 21-25].
Capsaicin
Capsaicin, via activation of vanilloid receptor-1 and release of calcitonin gene-related peptide from sensory neurons, upregulates IGF-1 and inhibits TGF-β, which induces apoptosis of keratinocytes through the phosphatidylinositol 3-kinase/Akt pathway [26]. Oral capsaicin 6 mg and isoflavone 75 mg daily for 5 months increased serum IGF-I in patients with AGA and AA in comparison to those who received placebo. Hair growth occurred in 64.5% of treated patients versus 11.8% of controls. In AGA specifically, 88% observed hair growth following treatment [26].
Capsaicin cream 0.075% applied daily to affected scalp in patients with extensive AA resulted in growth of vellus hairs at day 21 [27]. In addition, half of patients (12 AA and 2 AT) in a small prospective trial reported hair growth after three weeks of 0.075% topical capsaicin cream [28]. Comparing topical capsaicin ointment to clobetasol 0.05% ointment in 50 AA patients showed an improvement in vellus hair growth, but no significant cosmetic hair regrowth [29]. Further research shows that topical 0.01% raspberry ketone, which has a structure similar to capsaicin, also upregulates IGF-I and promotes hair growth in 50% of patients [30].
Curcumin
Curcumin, the active ingredient of turmeric, has been used for centuries as an anti-inflammatory agent. Curcumin downregulates cyclooxygenase-2, lipoxygenase, and inducible nitric oxide synthetase enzymes and inhibits nuclear factor-kB signaling, thereby decreasing proinflammatory cytokines such as tumor necrosis factor (TNF)-α and interleukin (IL)-1. Additionally, TNF-α and IL-1 are involved in follicular regression. Curcumin also has antioxidant, antimicrobial, antineoplastic, and antiandrogenic properties [31].
A 5% topical hexane extract of Curcuma aeruginosa (CA) was compared to placebo, 5% MXD, and combination CA and MXD in 87 patients. After 6 months, no significant improvement in total area hair count was noted in any group versus placebo. On photographic review, combination therapy and 5% MXD showed significant improvement, while subjective assessment of hair regrowth/shedding was only significantly improved in the combination group. While this study does not support the efficacy of CA extract alone for hair growth, it does suggest a synergistic effect when used in combination with MXD. In fact, CA has been shown to increase epidermal penetration of MXD, possibly improving drug delivery in AGA [32, 33].
Garlic Gel
Garlic (Allium sativum) belongs to the Allium genus along with onions, scallions, shallots, leeks, and chives. These plants produce organosulfur compounds, which have antimicrobial, immunomodulatory and anti-inflammatory effects [34]. In a trial of 40 AA patients, topical 5% garlic gel in combination with betamethasone was evaluated in comparison to placebo. After 3 months, good to moderate responses were observed in 95% of those treated compared to 5% with placebo. No adverse effects were reported [35]. Further investigation is needed to define the effect of topical garlic for hair loss.
Marine Proteins
Marine proteins, including extracellular matrix components from sharks and mollusks, have been produced for over 15 years to enhance hair growth. A Scandinavian researcher first described the exceptionally healthy skin and hair of the Inuit peoples to be a result of their fish- and protein-rich diet [36, 37]. Originally marketed as Hairgain® (Parexel, Norway) and later Viviscal® (Hair Nourishment System: Lifes2good, Inc., Chicago, IL, USA), marine peptide complexes are thought to enhance the proliferation of dermal papillae cells and increase levels of alkaline phosphatase, an indicator of anagen phase [38]. As summarized in a recent review, eight clinical trials and seven cohort studies demonstrated the ability of proprietary marine proteins, lipids, and glycosaminoglycans to promote growth of terminal and vellus hairs, increase hair shaft diameter, and decrease hair loss [36-51].
Two recent trials by Ablon and colleagues [50, 51] reported a significant improvement in hair counts and hair volume with the use of oral marine protein supplement (MPS). Using oral MPS 3 times daily in 100 females with self-perceived hair loss for 6 months demonstrated a significant increase in the mean hair diameter of vellus-like hairs, as well as a reduction in shedding [50]. Sixty males with AGA were treated with oral MPS twice daily for 6 months, resulting in significant increases in total hair count, total hair density, and terminal hair density, as well as fewer hairs extracted on the hair-pull test [51]. MPS appears to be an effective, well-tolerated CAM for patients with hair loss with no adverse events reported. Shellfish allergy is a contraindication to MPS use and detailed allergy history of prospective patients is warranted.
Melatonin
Melatonin is a neurohormone secreted by the pineal gland that regulates mammalian circadian rhythm. Melatonin is also an antioxidant synthesized in hair follicles [52]. The first study to report the effects of melatonin on hair growth compared topical melatonin 0.1% solution daily for 6 months in 40 patients with AGA or diffuse alopecia; efficacy was evaluated by trichograms to assess anagen and telogen hair. After treatment with melatonin, patients with diffuse alopecia had a significant increase in anagen hair at the occiput versus the frontal hairline [53].
A follow-up study evaluated a 0.0033% topical melatonin solution in an open-label study of 15 women and 15 men with AGA. After treatment, the degree of alopecia severity was significantly reduced. Using the same melatonin solution for 6 months in 35 men with AGA, TrichoScan evaluation demonstrated a 29.2% increase in the hair count in 54.8% of patients after 3 months, and a 42.7% increase in 58.1% of patients after 6 months. Hair density improved 29.1% in 54.8% of patients, and 40.9% in 58.1% of patients after 3 and 6 months, respectively. Continued research using 0.0033% topical melatonin solution, including a large multicenter study, demonstrated improvements in hair texture, decreased hair loss, and a reduction in seborrheic dermatitis [53, 54].
Onion Juice
Although the mechanism of topical onion juice in AA is unknown, it is thought that sulfur and phenolic compounds cause an irritant contact dermatitis, stimulating hair regrowth through antigenic competition. The effectiveness of topical crude onion juice in the treatment of AA compared to tap water was evaluated in 62 patients (45 treatment, 17 placebo). At 8 weeks 87% of patients treated with onion juice demonstrated full hair regrowth versus 13% using water. The most common reported adverse effect was unpleasant odor [55].
Procyanidin
Procyanidins are a class of flavonoids found mainly in plants, including apples, barley, cocoa, cinnamon, grapes, and tea, described to have antioxidant, anti-inflammatory and antifungal capabilities [56]. Procyanidins also induce anagen phase in murine hair models [57]. Topical 1% procyanidin B2, derived from apple juice, resulted in a significant increase in total and terminal hair counts at 4 months and 6 months in 29 patients with AGA compared to placebo [56, 58]. Procyanidin 0.7% used to treat 43 men with AGA also demonstrated a significant increase in hair counts (3.3 vs. –3.6 for placebo) after 6 months, with a total increase of 23 hairs/cm2 after 12 months [59].
Oral procyanidin supplementation (400 mg) was investigated in a double-blind, placebo-controlled randomized clinical trial (RCT) conducted in 250 patients with AGA. This procyanidin combination is extracted from Annurca, an apple variety native to Southern Italy with one of the highest contents of oligomeric procyanidins (specifically procyanidin B2). The supplement can be prepared with the addition of biotin, zinc, and selenomethionine (AMSbzs) or without (AMS). Both supplements lead to improvement in all hair clinical parameters, with the AMSbzs cohort demonstrating increased hair density by 125.2%, hair weight by 42.1%, and keratin content by 40.1% at 2 months [60]. Procyanidins also upregulate MAPK/extracellular signal-related kinase kinase (MEK) in hair epithelial cells and counteract hair growth inhibitory effects of TGF-β in vitro, which may account for these clinical results [61, 62]. Additional studies are warranted to further define the effect of procyanidins on hair growth.
Pumpkin Seed Oil
Pumpkin (Cucurbita pepo) is a member of the squash family native to North America. Pumpkin seed oil (PSO) contains phytosterols known to inhibit 5α-reductase, preventing the conversion of testosterone to active dihydrotestosterone (DHT) [63]. Comparing 400 mg of oral PSO daily to placebo for 24 weeks in 76 patients with AGA demonstrated a mean increase in hair count of 40 versus 10% with placebo, with improved patient-reported satisfaction scores. However, this PSO Korean supplement (Octa Sabal Plus®; Serona Company, South Korea) contains additional ingredients derived from mixed vegetables, primrose, red clover, and tomatoes, making it unclear whether the effects are due mostly to the PSO component [64]. In addition, this study showed that PSO is a promising treatment for AGA involving the vertex, but failed to address the supplement’s effect on frontal variants. Additional studies are required to confirm these preliminary results of the effects of PSO on hair growth.
Rosemary Oil
Rosemary (Rosmarinus officinalis L.) is an aromatic evergreen herb with antioxidant, antibacterial, antifungal, and anti-inflammatory properties [65]. Rosemary also enhances microcapillary perfusion. In an RCT with 100 AGA patients, topical rosemary oil lotion (3.7 mg/mL) applied daily was noninferior to topical 2% MXD. Both groups demonstrated a significant increase in hair count at 6 months. The most common adverse effect reported was scalp itching, more frequent with MXD use [66]. Rosemary oil appeared to be a safe nonprescription alternative for AGA, and the results of this study merit further investigation.
Saw Palmetto
Saw palmetto (SP, Serona repens) is an extract from the berries of the saw palmetto palm tree (American dwarf tree) containing phytosterols (β-sitosterol), fatty acids, β-carotene, and polysaccharides. SP is a competitive, nonselective inhibitor of both forms of 5α-reductase. SP blocks nuclear uptake of DHT in target cells and decreases DHT binding to androgen receptors by approximately 50%. Additionally, the extract increases 3α-hydroxysteroid-dehydrogenase activity, increasing the conversion of DHT to its weaker metabolite, androstanediol. As a result, the pharmacodynamic profile of SP differs from finasteride due to multiple sites of action [67, 68].
Twenty-six males with AGA treated with either 50 mg of oral β-sitosterol and 200 mg SP or placebo daily resulted in 60% of patients with “improved” outcomes compared to 11% of controls. Gastrointestinal side effects, including loss of appetite, flatulence, and diarrhea, were experienced by 3 patients [69]. In another study, 100 men with AGA were treated with 320 mg of oral SP extract or 1 mg of oral finasteride daily for 2 years. Although hair growth scores were higher in the finasteride group with 68% experiencing growth at the front and vertex of scalp, 38% of patients in the SP cohort also had an increase in hair growth, mainly on the vertex [70].
In addition to systemic therapy, SP has also been studied as a topical agent. A study evaluating the hair growth effect of 3.3 mL topical SP serum applied for 4 weeks and 2 mL lotion for 24 weeks, in 50 men with AGA, demonstrated increased average and terminal hair counts at 12 and 24 weeks [71]. Although systemic SP has not demonstrated superiority to conventional systemic therapies, it does have clinical benefits and is an attractive alternative treatment for male AGA patients who are not interested in oral finasteride.
Vitamin B7 (Biotin)
Biotin, also known as vitamin B7 or vitamin H, is a B-complex vitamin and cofactor for carboxylase enzymes involved in fatty acid synthesis, amino acid catabolism, gluconeogenesis, and mitochondrial function in hair root cells [72]. Deficiency causes various symptoms, including alopecia, dermatitis, conjunctivitis, candidiasis, ataxia, seizures, hypotonia, developmental delay, and hearing and vision loss [72, 73].
Biotin deficiency (< 100 ng/L) and suboptimal biotin levels (100–400 ng/L) were reported in 38% and 49% of healthy women complaining of hair loss, respectively. However, 11% of these patients were later found to have a secondary cause for low biotin levels, including use of antiepileptics, isotretinoin, antibiotics, or gastrointestinal disease altering the biotin-producing gut microflora [74].
Although highly popularized in the media for its beneficial effects on hair loss, there have been no RCTs to evaluate the effect of biotin supplementation in alopecia [75]. Patients taking isotretinoin or valproic acid have decreased biotinidase levels, the enzyme responsible for releasing biotin from food. As a result, isotretinoin-associated TE and alopecia secondary to valproic acid may benefit from biotin supplementation [76, 77]. A recent review identified 11 cases of hair loss secondary to biotin deficiency, from either an inherited enzyme deficiency or medication, where biotin was an effective supplementation for hair regrowth [78]. Current clinical evidence supports biotin supplementation as an effective CAM for hair loss only in cases secondary to biotin deficiency; however, apart from medications, this is rare in developed countries due to well-balanced dietary intake [79].
Clinicians should exercise caution in recommending biotin as an oral supplement for hair loss because it may interfere with thyrotropin and thyroid hormone assays, resulting in artificially high or low thyroid function results [80]. Many immunoassays used in diagnostic tests rely on the binding of biotin with streptavidin to improve test sensitivity; high levels of serum biotin can compete with these immunoassays. Multiple cases have been reported in which patients taking high levels of biotin had laboratory results indistinguishable from Graves disease, and as a result were unnecessarily treated with antithyroid medications [81, 82]. Biotin may also interact with troponin, N-terminal pro-brain natriuretic peptide, and parathyroid hormone assays, underscoring the need for a comprehensive medication history at every patient visit, including the use of over-the-counter supplements [83].
Vitamin D
Vitamin D is a fat-soluble molecule that plays an important role in calcium and phosphorus homeostasis, as well as immune regulation. Vitamin D dysregulation may contribute to autoimmune diseases, including rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis [84]. Vitamin D receptors are intracellular receptors expressed in hair follicles, essential for normal hair cycle and differentiation of the interfollicular epidermis. Homozygous knockout of vitamin D receptor in mice resulted in the development of alopecia and near total hair loss at 8 months [85].
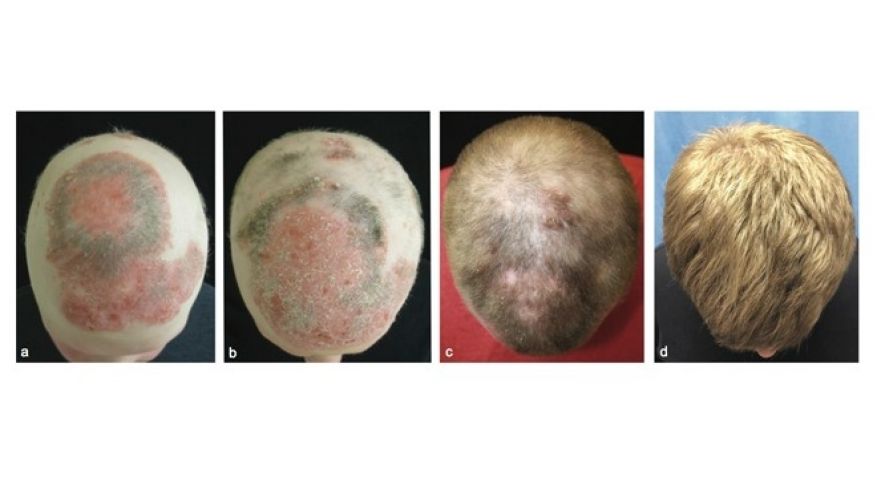
Meta-analyses have reported that AA patients have a higher prevalence of vitamin D deficiency and lower 25-hydroxyvitamin D serum levels compared to healthy controls [86]. One study reported the presence of vitamin D deficiency in 39% of AA patients compared to 12.79% of healthy controls [87]. Given this association, multiple studies have investigated the efficacy of oral vitamin D supplementation for AA treatment; however, they failed to support its benefit in AT/alopecia universalis (AU) or its ability to potentiate squaric acid dibutylester [88, 89]. A case report of presumed AA associated with reduced vitamin D receptor expression reported a complete clinical remission after topical calcipotriol ointment 50 μg/mL applied once daily for 3 months [90]. AA patients using topical 0.005% calcipotriol cream twice daily for 12 weeks had greater than 50% hair regrowth in 65% of patients, greater than 75% hair regrowth in 62.5% of patients, and complete regrowth in 27.1% [91]. Twice daily topical 0.005% calcipotriol in 22 patients with patchy AA resulted in 59.1% of patients demonstrating hair growth within 4.21 ± 2.13 weeks. Patients with lower baseline serum vitamin D levels responded faster and more robustly [92]. Studies using topical vitamin D in alopecia are inconsistent and limited by small sample size or lack of appropriate controls. Preliminary results suggest a potential therapeutic benefit for topical vitamin D, with minor side effects [88-92].
Vitamin E Derivatives (Tocotrienols)
Vitamin E consists of fat-soluble compounds known as tocopherols and tocotrienols that function as antioxidants by scavenging peroxyl radicals [93]. Eight months of supplementation with 50 mg of mixed tocotrienols and 23 IU of α-tocopherol resulted in 34.5% increased hair count in 38 patients with hair loss, compared to a 0.1% decrease with placebo. The ability of the derivatives to inhibit lipid peroxidation may limit hair follicle oxidative stress, thus preventing hair loss; however, additional studies are needed [94].
Zinc
Zinc is an essential trace element involved in enzyme catalysis, protein folding, and gene expression. Signs of deficiency include growth retardation, delayed puberty, diarrhea, alopecia, glossitis, nail dystrophy, and decreased immunity among others [95]. Low zinc levels have been identified in patients with AA, AGA, and TE [96]. Proposed mechanisms for zinc-associated hair regrowth include antimicrobial, anti-inflammatory, antioxidant, and anti-5α-reductase activity [97-100]. Zinc has been studied as both a topical and oral supplement.
Zinc chelates with pyrithione to create a coordination complex that acts as an antifungal for treatment of seborrheic dermatitis [101]. Comparing the efficacy of 1% pyrithione zinc shampoo used daily, 5% topical MXD solution used twice daily, or a combination of both, for 9 weeks in 200 AGA patients resulted in increased hair counts in all groups compared to placebo. However, the 1% pyrithione zinc group had only a modest improvement in hair growth, with hair counts less than half of the MXD group. No increase in hair count was noted between the combination therapy versus MXD alone [102].
Oral supplementation of zinc has been studied for AGA and AA. Supplementation of 50 mg of zinc sulfate daily, 100 mg of calcium pantothenate (the calcium salt of vitamin B5) daily, or a combination of the two twice weekly was compared to 2% topical MXD solution in 73 women with AGA, demonstrating positive outcomes in all groups. Although 2% MXD results in a greater increase in hair density, oral zinc and pantothenate supplementation creates thicker hair shafts [103].
AA may present with concomitant zinc deficiency, and oral supplementation may be beneficial at a dose of 50 mg daily, with positive results seen in 67% of patients in one study and complete resolution seen in a child with diffuse alopecia [104, 105]. In a double-blinded, cross-over study, researchers systematically evaluated oral zinc sulfate (5 mg/kg/day) for the treatment of AA in 100 patients. The first cohort was initially treated with zinc and then placebo, resulting in complete hair regrowth in 60% of patients after 3 months and maintenance for 3 months after cessation. Conversely, the second cohort was first treated with placebo and then zinc. After 3 months of placebo, 10% of patients completely regrew hair, and subsequent supplementation with zinc resulted in 67% of patients with complete regrowth. Side effects were mild, including gastric upset [106]. Topical and oral zinc supplementation may prove to be an efficacious adjuvant for both AGA and AA treatment in patient populations that would like CAM modalities.
Mind and Body Medicine
Mind and body medicine focuses on the connection between the brain, body, and behavior, utilizing techniques administered by trained practitioners and teachers to reduce physiologic stress and subsequent detri mental health effects [107]. Of the variety of techniques available, acupuncture, aromatherapy, massage, hypnotherapy, and psychotherapy have been studied for the treatment of hair loss.
Acupuncture
Acupuncture involves the insertion of fine needles at specific points for therapeutic purpose, with ample evidence for benefit in back pain, osteoarthritis, and migraines [108]. Plum-blossom acupuncture, which uses seven needles arranged in the shape of a flower, is used to treat a number of dermatologic diseases [109].
It is thought that acupuncture can increase circulation, stimulate hair follicles, and decrease inflammatory infiltrates [110]. In a murine model of AA, electroacupuncture (acupuncture with low electric current) reduced degranulation of mast cells in the dermis and improved hair growth [111]. Complete regrowth of hair occurred in 89% and marked improvement in 11% of AA patients receiving acupuncture [112]. Seventy-eight patients were treated with either plum-blossom acupuncture of the alopecia area or topical 2% MXD daily with total hair regrowth in 58.1% of acupuncture patients versus 34.3% of MXD patients [113]. In a Korean case report, combining acupuncture, pharmacopuncture, and needle-embedding resulted in an unspecified “remarkable” improvement of AGA [114]. Additional studies are necessary to clearly elucidate the role of acupuncture in hair loss treatment.
Aromatherapy/Massage
Aromatherapy uses essential oils from plants with demonstrated benefit in the treatment of several dermatologic diseases [115, 116]. Cedarwood, lavender, thyme, and rosemary oils have been used anecdotally for over 100 years to treat hair loss [98-99]. Massaging these essential oils, in jojoba and grape seed carrier oils, into the scalp of 84 AA patients for 7 months demonstrated significant improvement in hair growth in 44% of patients, compared to 15% of patients massaged with both carrier oils alone [115]. Further, there is a case of AA responding to a combination of massage and relaxation, with full hair growth [117]. Current evidence for use of aromatherapy and massage in hair loss is lacking and additional studies are warranted to control for confounding effects.
Hypnotherapy
Hypnotherapy has been explored as a potential treatment for hair loss. The patient is brought into a trance-like state of consciousness, involving heightened concentration and attention, with increased responsiveness to suggestion from the therapist, thus dealing directly with the subconscious mind [118]. Hypnotherapy techniques (direct and indirect suggestion, ego strengthening) used for the treatment of AA have conflicting results, from studies with clearly no response [119, 120] to those demonstrating positive results [118]. One study reported an improvement in anxiety and depression after 10 hypnotherapy sessions in 20 AA patients over 6 months – however, not in hair loss [120]. After three to eight sessions in 21 patients (9 AT/AU and 12 AA), 57% of patients had significant hair regrowth and 42% patients had total hair regrowth. Anxiety and depression scores improved in all patients. Of the patients who responded to hypnosis, 3 used no additional conventional therapy and 8 used concomitant corticosteroids or immunotherapy. Relapse occurred in 5 patients after cessation of hypnosis [118].
Psychotherapy
The term psychotherapy is derived from the Greek psyche meaning “breath, spirit, soul” and therapaia meaning “healing, medical treatment” [121]. In contrast to hypnotherapy, psychotherapy works directly on the conscious state of mind. Overall, the evidence for psychotherapy in the treatment of hair loss is promising, yet limited. The addition of relaxation and image therapy for 30 min weekly for 2 months as a complementary treatment to immunotherapy (prednisolone 5–10 mg/day for 2 months, followed by cyclosporine 2.5 mg/kg and prednisolone for another 4–5 months) resulted in hair growth in 83% of refractory AU patients, compared to 17% of patients experiencing regrowth with immunotherapy alone [122].
Other
The group referred to as “other” is comprised of Ayurvedic medicine, traditional Chinese medicine, homeopathy, naturopathy, and practices of traditional healers [1, 2]. Electromagnetic stimulation, homeopathy, and traditional Chinese medicine have been evaluated for the treatment of hair loss. Electromagnetic stimulation uses a magnetic field to generate electric current flow in a small area of the brain. This therapy is beneficial in treating neuropathic pain, as well as major depressive disorder [123, 124]. Transcranial magnetic stimulation was evaluated as a therapeutic modality for AA when researchers noticed hair regrowth in a 6-year-old girl with AA and epilepsy after treatment with external magnetic field therapy. Low-intensity transcranial magnetic stimulation 5 times per week on 3 AU patients resulted in hair regrowth [125, 126]. Combining essential oils with low-intensity electromagnetic pulses for 26 weeks in 69 AGA patients as part of a double-blind clinical trial demonstrated significant improvement in hair counts in the treatment group compared to controls. No adverse events have been reported with magnetic stimulation [127].
Homeopathy is an alternative medicine system based on the controversial doctrine “like cures like,” in which a substance that causes disease in a healthy person would conversely cure disease in a sick person [128]. It involves the dilution of a certain substance to a nondetectable concentration for therapeutic benefit and has been used in a variety of dermatologic diseases, including atopic dermatitis, acne, chronic urticarial, psoriasis, and alopecia [129]. A 20-year-old female with AU was treated with Mercurius (derived from the highly toxic mercury, but reportedly safe at low concentrations in homeopathy preparations) for 3 months, resulting in a 75% improvement according to the patient’s own self-assessment. Although no adverse effects were reported in that case, we as authors are not comfortable recommending this treatment modality [129]. Finally, the use of a traditional Chinese concoction, made of various plant roots, both topically and orally for 3 months, stimulated hair growth in an 11-year-old girl with a year and a half history of AA [130].
The Need for CAM in Hair Loss
Hair loss is a disorder with significant adverse psychological effects, including low self-esteem, low confidence, and negative influence on social interactions; 52% of women and 28% of men report being very to extremely upset by their alopecia [131]. As a result, patients who do not see significant improvements in hair growth with conventional therapy often turn to CAM.
AGA, also known as male or female pattern hair loss, is the most common form of hair loss, affecting up to 50% of the adult male and 40% of the adult female population [132, 133]. Current FDA-approved treatment options for hair loss are limited to topical MXD (for men and women), oral finasteride (men only), and low-level light therapy (men and women). Unfortunately, all therapies are limited by their incomplete efficacy and risk of recurrence after cessation [134, 135]. Side effects related to MXD include facial hypertrichosis in 3–5% of women and contact dermatitis in 6.5% of patients [132, 136, 137]. Systemic finasteride also boasts a large adverse effect profile including sexual dysfunction and post-finasteride syndrome with associated depression and/or psychosis [138, 139]. More invasive procedures for hair restoration include hair transplantation surgery or injections of platelet-rich plasma, which are costly, time-consuming, and require multiple treatment sessions.
AA is a chronic, and often recalcitrant, disorder characterized by nonscarring hair loss secondary to collapse of immune privilege at the hair follicle, with a lifetime prevalence of approximately 2% [140, 141]. There are no FDA-approved treatments for AA and evidence for current treatments targeting inflammation or immune dysregulation is limited. Corticosteroids can be administered orally, topically, or as intralesional injections; however, they have only short-term benefit and systemic use is associated with multiple adverse effects [142]. Other treatment options include systemic immunomodulation (cyclosporine, methotrexate), ultraviolet light (PUVA), topical MXD, topical immunotherapy (diphencyprone [DPCP], anthralin, squaric acid) and off-label use of Janus kinase (JAK) inhibitors both systemically or topically. These therapies are limited by lack of efficacy and potential serious adverse events. No therapy has yet demonstrated sustained, long-term benefit for AA patients.
CAMs boast the ability to “cure” hair loss “safely” with “less side effects” than conventional medicine. However, it is important for both clinicians and patients to look beyond the overarching claims and marketing to critically review the literature. Some CAMs have evidence as hair loss therapies, backed by RCTs, while others have little evidence. Inherently, it is difficult to test the efficacy of CAM as adjuvants, as they are often used in conjunction with conventional therapies or as combinations with each other. Given the growing interest in CAM for multiple diseases, including hair loss, there is a need for additional studies with robust clinical design and reproducible, quantitative measures with noninvasive imaging techniques.
Conclusion
There are a variety of CAMs on the market for alopecia; however, only a few are backed by strong clinical evidence. Clinicians should be aware of these products, the marketing strategies used to promote said products, expected clinical outcomes, and side effect profiles to ensure accurate patient counseling. As with any medical history, it is always important to be thorough and include over-the-counter vitamins, minerals, and supplements. It is also important to elicit a complete allergy history as some allergies may preclude the use of certain CAMs. In addition, CAMs may cause further scalp inflammation, such as irritant or contact dermatitis, leading to more hair loss. Given the growing interest in CAMs for multiple dermatologic conditions including alopecia, it is important for clinicians to stay up to date and practice evidence-based medicine when recommending CAMs.
[“source=karger”]